Hey everyone, doc Miles at North American Rescue. I'm going over some of the uses of prehospital ultrasound to help guide care in patients. So one area that ultrasound can be particularly useful is determining whether or not your patient has a pneumothorax.
Differential Diagnosis: Hemorrhagic Shock or Tension Pneumothorax?
So sometimes it can be confusing. Is my patient crashing because they've got a tension pneumothorax, or is it because they've got hemorrhagic shock? Well, we want to do the right treatment for the right problem. So if we don't need to needle decompress the chest, then no reason to, let's get on with resuscitation. Hemorrhagic shock, right?
So today I am using the Butterfly IQ 3, which is a great prehospital ultrasound, running into my iPhone. I'm going to start scanning a few different sites on the chest. Different protocols call for different spots, but all we're going to do is we're going to look at the chest, we're going to go perpendicular down, and then as I'm looking at my ultrasound, I'm going to see ribs and those are going to cause a shadow between the ribs.
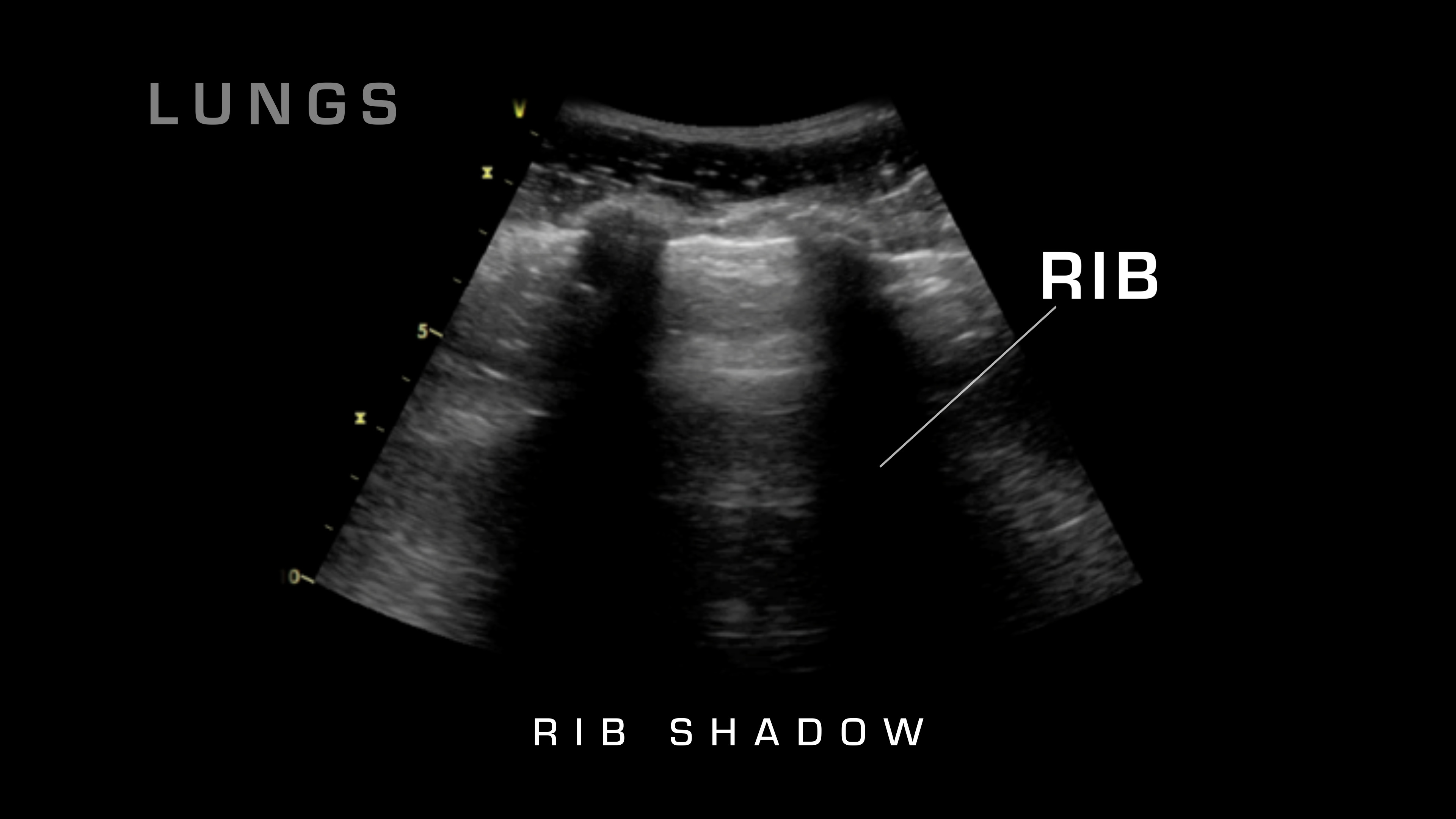
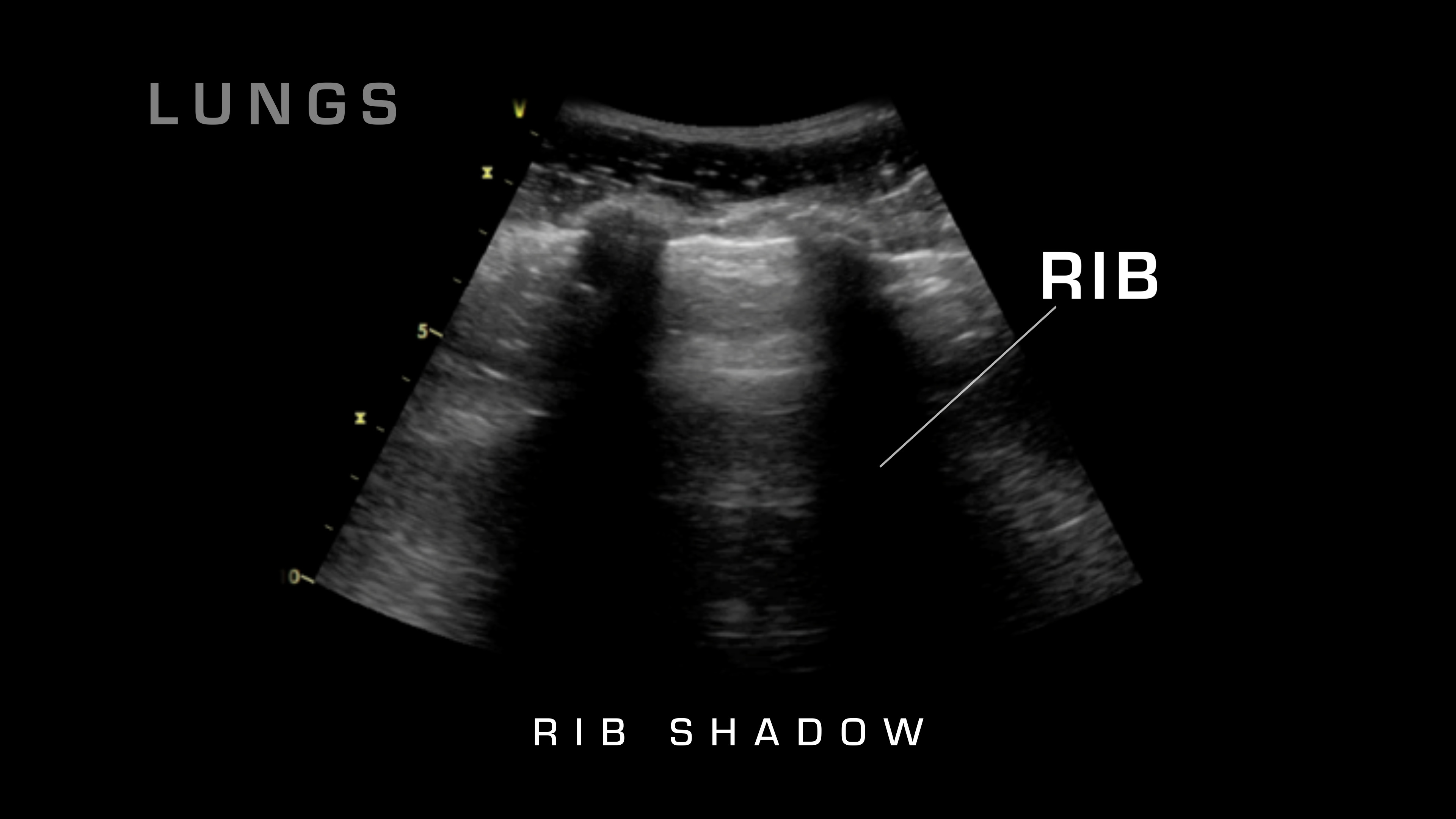
I can really get a good evaluation of the lung. So what am I looking for between the lungs? Well, I'm looking for lungs sliding. Basically what you'll see is at that parietal pleura, as it hits the chest wall, you're going to see lungs sliding back and forth with normal respiration. If you don't see that, then you are missing lung sliding, and that's an indication of a pneumothorax.
As you go and scan the different areas, you may find what's called a lung point. A lung point is where you will see lungs sliding on one portion and then you'll see it stop sliding on the other. And that's how you know where you're at on a pneumothorax. So basically you see normal to pneumothorax and that's the start of your pneumothorax.
Ultrasound Guided Needle Decompression
So one of the other advantages of using an ultrasound to diagnose and treat tension pneumothorax prehospital is that I can actually use it to do an ultrasound guided needle decompression. Once I've determined my location, I'm going to make sure I can see that lung tissue, and then what I can do is I can go in at the proper spot and actually watch it on ultrasound as that needle penetrates in into the pleural space. That way I ensure that I've gone far enough into penetrate, into the thoracic cavity, into the pleural space, and now I've done an effective needle decompression.